EFFICACY


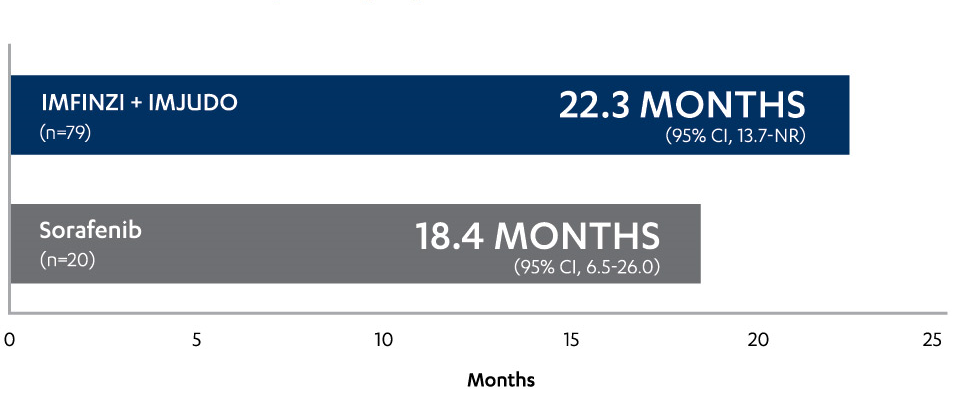
STATISTICALLY SUPERIOR OS (primary analysis)1-3
Median duration of follow-up was 33.2 months (range: 31.7-34.5) for IMFINZI + IMJUDO and 32.2 months (range: 30.4-33.7) for sorafenib. Data cutoff: August 27, 2021.
NEW 5-YEAR OS UPDATE (post-hoc analysis)4†
†In the post-hoc analysis, median duration of follow-up was 62.5 months (range: 59.5-64.8) for IMFINZI + IMJUDO and 59.9 months (range: 58.3-61.5) for sorafenib. OS data maturity across the IMFINZI + IMJUDO and sorafenib arms was 82%. Data cutoff: March 1, 2024.
IMFINZI + IMJUDO set the 5-year benchmark for OS data with a 1L dual-IO regimen in uHCC1-4,7-10
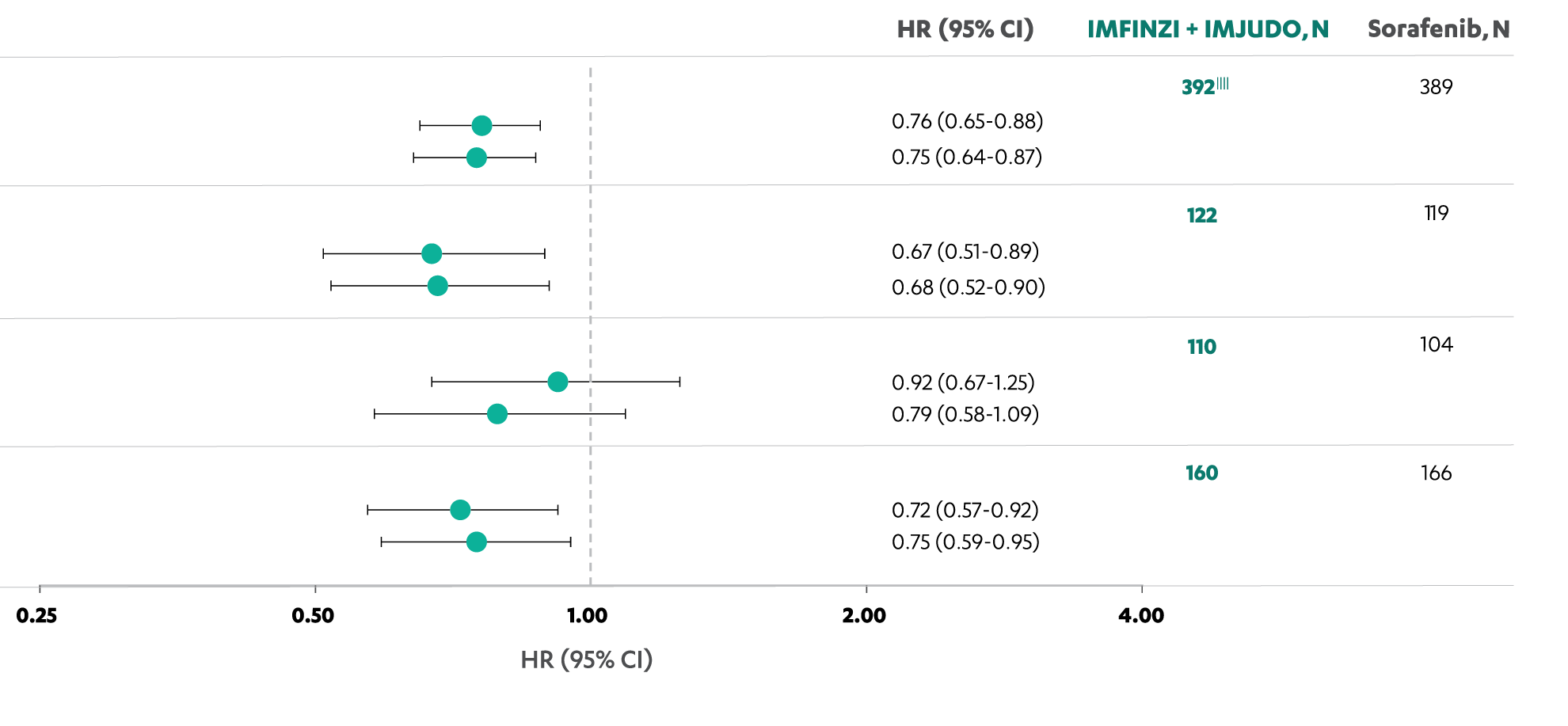
IMFINZI + IMJUDO demonstrated consistent OS data across most prespecified subgroups
OVERALL SURVIVAL BY PRESPECIFIED SUBGROUP (post-hoc analysis)4,11
SCROLL
For all patients, OS HRs and 95% CIs were calculated using a Cox proportional hazard model adjusting for treatment, etiology, ECOG PS, and MVI. For the subgroup analysis, the HR and 95% CI were estimated from an unstratified Cox proportional hazard model with treatment as the only covariate and using the Efron method to control for ties.4,11
‡Stratification factors.
This updated 5-year post-hoc analysis represents the longest follow-up among positive Phase III studies to evaluate IO therapy as 1L treatment of uHCC1,2,4,11§
§Median duration of follow-up was 62.5 months (range: 59.5-64.8) for IMFINZI + IMJUDO and 59.9 months (range: 58.3-61.5) for sorafenib.4
Post-hoc analysis; not powered for statistical significance5
5-YEAR OS DATA BY BASELINE ALBI GRADE (post-hoc analysis)5||
||Data cutoff: March 1, 2024.
¶ALBI grade data not available for 1 participant.
#One participant in the IMFINZI + IMJUDO arm and 1 participant in the sorafenib arm were classified as ALBI Grade 3 at baseline.
Adapted from Kudo M, et al. 2024.
ALBUMIN-BILIRUBIN (ALBI) GRADING6
| ALBI Grade | Score | Level of liver decompensation/ dysfunction |
|---|---|---|
| 1 | ≤-2.60 | Mild liver decompensation/ dysfunction |
| 2 | >-2.60 to ≤-1.39 |
Moderate liver decompensation/ dysfunction |
| 3 | >-1.39 | Severe liver decompensation/ dysfunction |
BASELINE DISEASE ETIOLOGY3
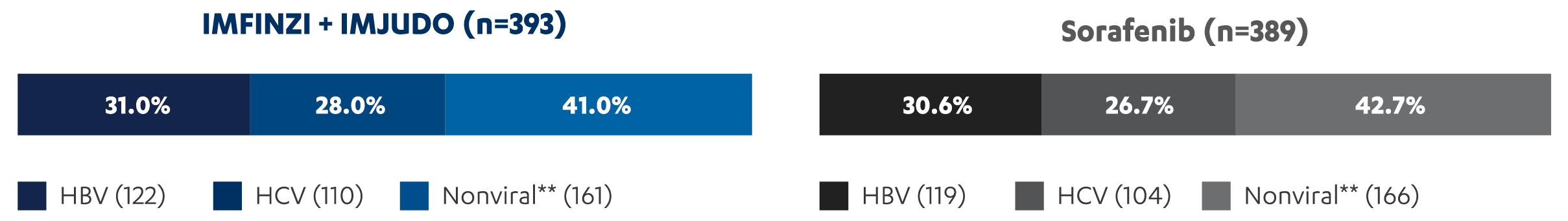
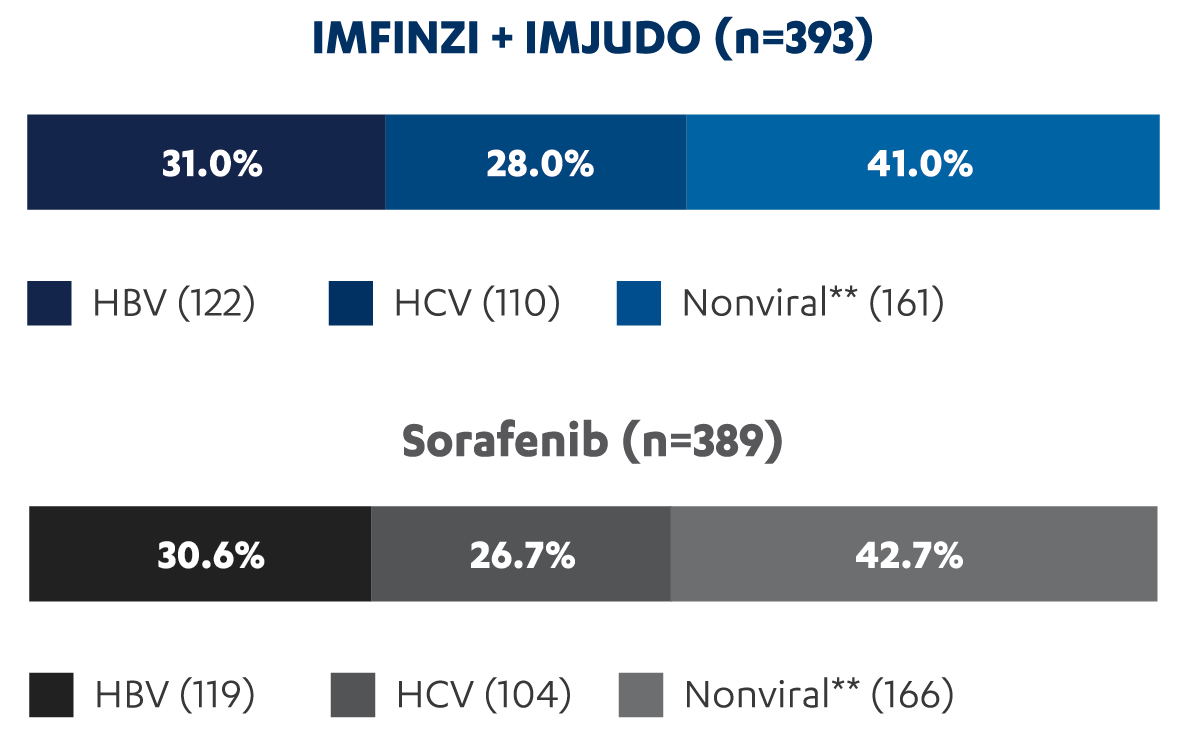
**No active viral hepatitis identified.
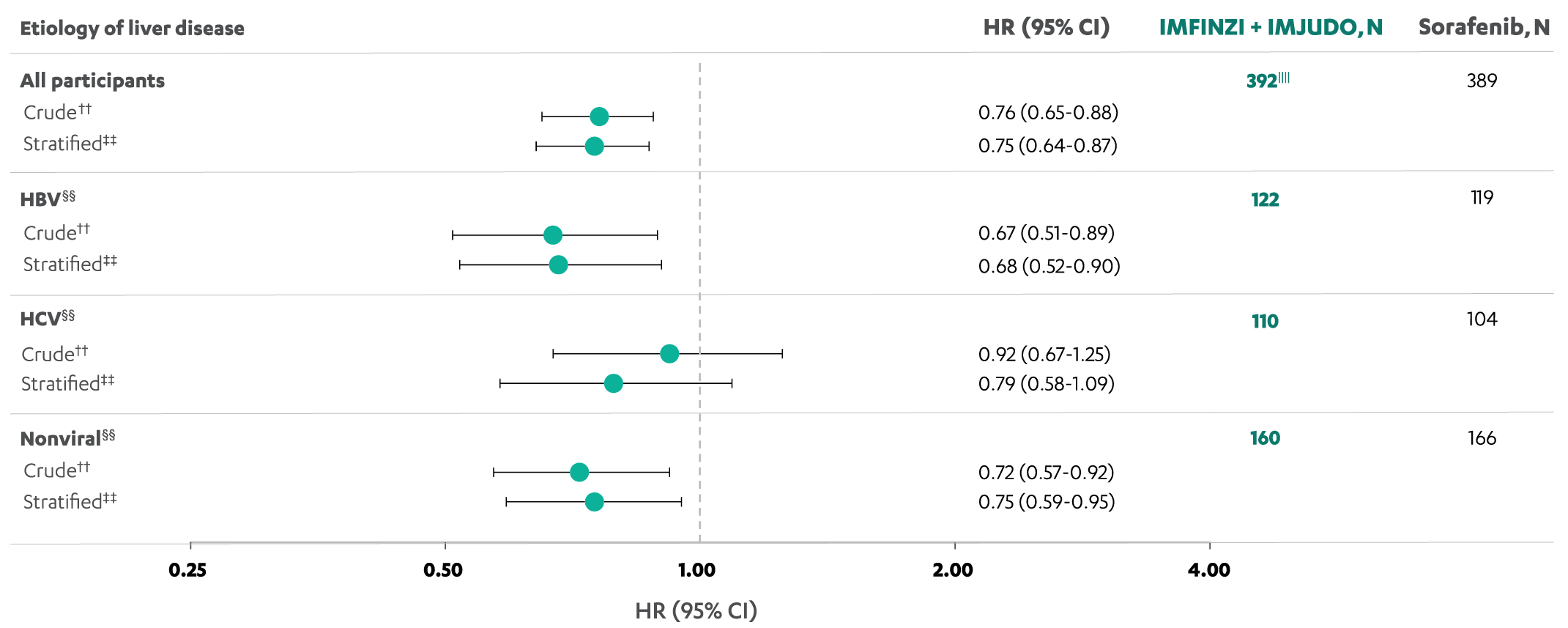
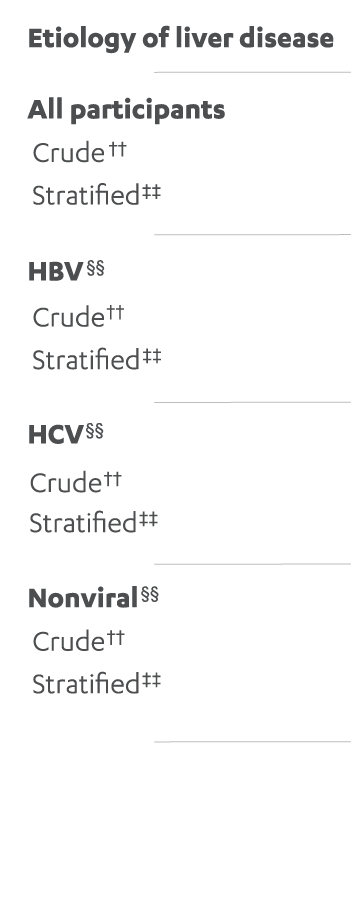
Overall survival results at 5 years were consistent across etiological subgroups4,11
5-YEAR OS RESULTS BY ETIOLOGY (post-hoc analysis)
 |
 |
|---|
SCROLL
††The hazard ratio and 95% CI from the crude model are estimated from an unstratified Cox proportional hazards model with treatment as the only covariate and using the Efron method to control for ties.
‡‡The hazard ratio and 95% CI from the stratified model are estimated from a stratified Cox proportional hazards model adjusting for EHS (no vs yes/missing), ALBI grade (1 vs 2/3), and using the Efron method to control for ties.
§§Values of etiology of liver disease (HBV vs HCV vs others/nonviral) are obtained from the pathology at screening.
||||One participant was removed due to missing ALBI score.
A post-hoc analysis was performed to characterize the patients surviving ≥48 months after randomization¶¶
CHARACTERISTICS OF PATIENTS TREATED WITH IMFINZI + IMJUDO AT THE 5-YEAR UPDATE AND AT BASELINE IN THE FULL ANALYSIS SET (post-hoc analysis)4,11
HBV: Patients who tested positive for HBsAg or anti-HBcAb with detectable HBV DNA. HCV: Patients who tested positive for HCV or had a history of HCV infection. Nonviral: No active viral hepatitis identified. Viral etiology, MVI, and/or EHS determined at screening. BCLC determined at study entry.
¶¶Data cutoff: March 1, 2024.4,11
In the IMFINZI + IMJUDO arm, characteristics of patients at the 5-year update were generally consistent with those of the population at baseline4,11
Not powered for statistical significance.
In the first-line treatment of unresectable HCC
CONFIRMED OBJECTIVE RESPONSE RATE IN THE
INTENT-TO-TREAT POPULATION (secondary endpoint)1-3*
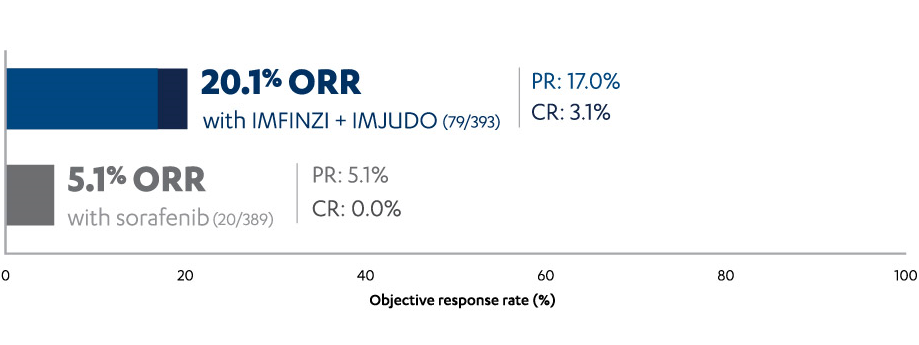
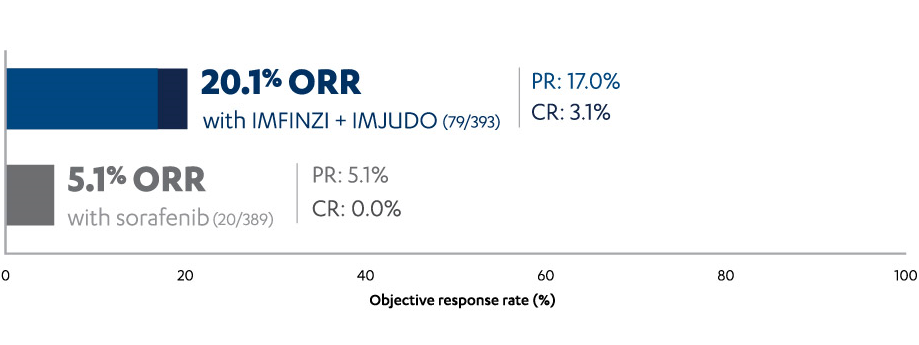
*Based on Clopper-Pearson method.
†Disease control rate is the sum of complete response rate, partial response rate, and stable disease rate.3
‡The HR is based on the stratified Cox proportional hazard model.1,2
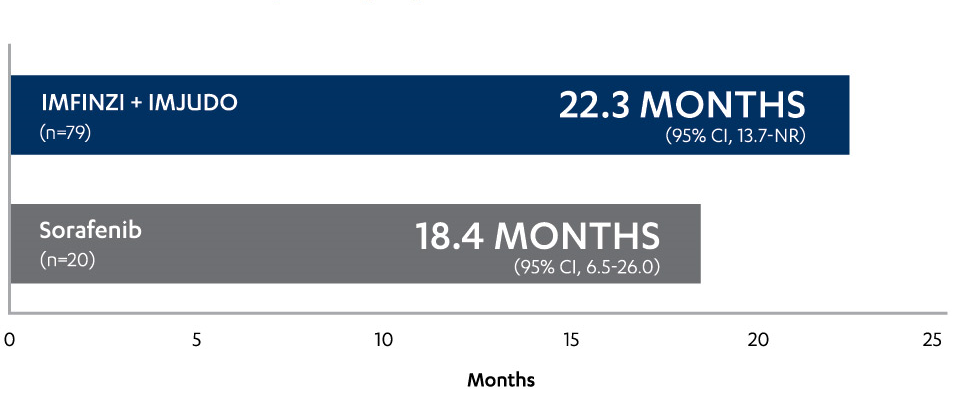
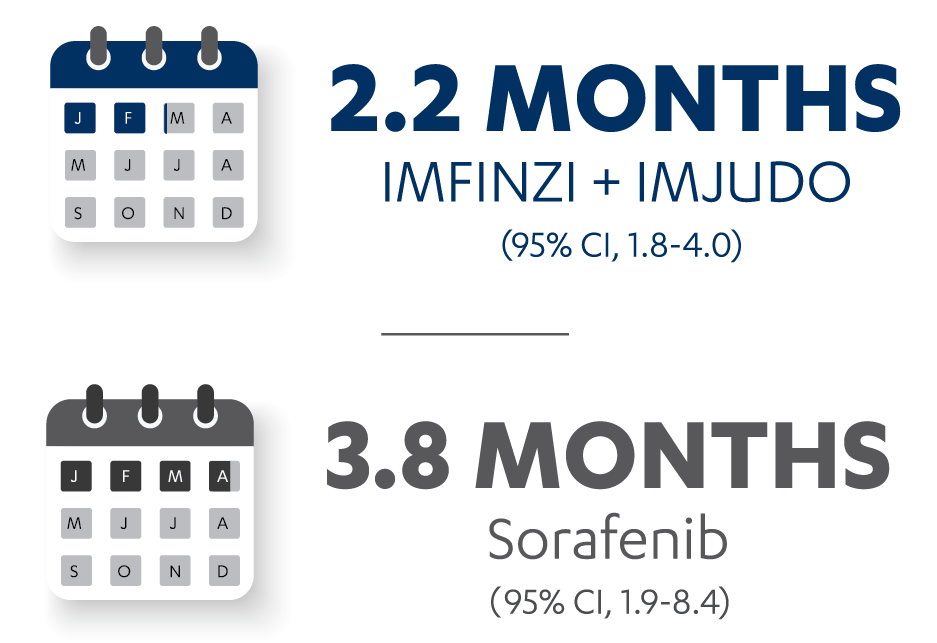
MEDIAN DURATION OF RESPONSE
(secondary
endpoint)1-3
MEDIAN TIME TO RESPONSE
(secondary endpoint)3

STRIDE (Single Tremelimumab Regular Interval Durvalumab) is the name given to the IMFINZI + IMJUDO regimen evaluated in the HIMALAYA study3
STUDY DESIGN: PHASE III, OPEN-LABEL, MULTICENTER, GLOBAL STUDY1-3
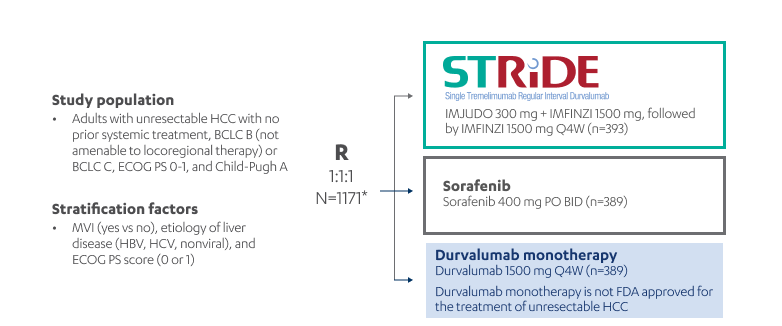
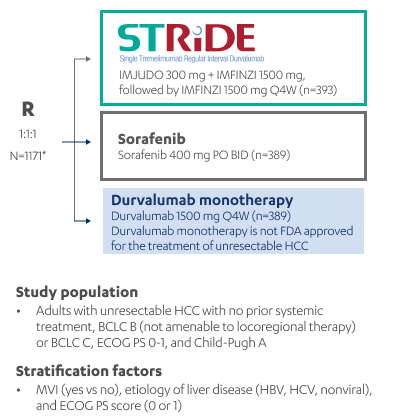
Treatment continued until disease progression or unacceptable toxicity. Patients in all arms could continue to receive treatment after evidence of disease progression if, in the investigator’s opinion, they were still benefiting from treatment and continued to meet inclusion and exclusion criteria.
*The HIMALAYA study included an additional arm of therapy: The IMJUDO 75-mg + IMFINZI arm (n=153) was closed following a preplanned analysis of a Phase II study. Results from this arm are not reported in this material, and this dosing regimen is not approved for use.3
The HIMALAYA study included patients with BCLC B or C disease, ECOG PS 0 or 1, and Child-Pugh A classification3
![]() No EGD required to initiate therapy in the HIMALAYA study1-3‡
No EGD required to initiate therapy in the HIMALAYA study1-3‡
†PFS, ORR, and DoR were investigator assessed according to RECIST v1.1. Tumor assessments were conducted every 8 weeks for the first 12 months and then every 12 weeks thereafter.1-3
‡No EGD was required to screen for esophageal varices for trial eligibility. Patients with active or prior documented GI bleeding within 12 months were excluded. For patients with a history of GI bleeding for greater than 12 months or assessed as high risk for esophageal variceal, adequate endoscopic therapy was required.1-3
Patient demographics and disease characteristics were well balanced between arms3
BASELINE DEMOGRAPHICS AND DISEASE CHARACTERISTICS3
| Patient characteristics | IMFINZI + IMJUDO (n=393) | Sorafenib (n=389) |
|---|---|---|
| Median age, years (range) | 65 (22-86) | 64 (18-88) |
| Sex, n (%) Male Female |
327 (83.2) 66 (16.8) |
337 (86.6) 52 (13.4) |
| Region, n (%) Asia (excluding Japan) Rest of world (including Japan)§ |
156 (39.7) 237 (60.3) |
156 (40.1) 233 (59.9) |
| ECOG PS score, n (%) 0 1 2 |
244 (62.1) 148 (37.7) 1 (0.3) |
241 (62) 147 (37.8) 1 (0.3) |
| Child-Pugh classification, n (%) A/5 A/6 B/7 Others|| |
295 (75.1) 92 (23.4) 4 (1) 2 (0.5) |
277 (71.2) 102 (26.2) 10 (2.6) 0 |
| BCLC stage, n (%) B C |
77 (19.6) 316 (80.4) |
66 (17) 323 (83) |
| Etiology, n (%) HBV HCV Nonviral¶ |
122 (31) 110 (28) 161 (41) |
119 (30.6) 104 (26.7) 166 (42.7) |
| MVI, n (%) | 103 (26.2) | 100 (25.7) |
| EHS, n (%) | 209 (53.2) | 203 (52.2) |
| AFP ≥400 ng/mL, n (%) | 145 (36.9) | 124 (31.9) |
| Prior disease-related radiotherapy, n (%) | 48 (12.2) | 37 (9.5) |
| PD-L1 status, n (%)# Positive Negative Missing |
148 (37.7) 189 (48.1) 52 (13.2) |
148 (38) 181 (46.5) 45 (11.6) |
SCROLL
§Includes Brazil, Canada, France, Germany, Italy, Japan, Russia, Spain, Ukraine, and the United States.
||None of the above.
¶No active viral hepatitis identified.
#Baseline PD-L1 results were not available for patients who were randomized but not treated. PD-L1 expression level was based on the tumor and immune cell positivity score method as PD-L1 positive (≥1%) or negative (<1%).


IMFINZI is indicated for the treatment of adult patients with unresectable Stage III non-small cell lung cancer (NSCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy.
IMFINZI, in combination with IMJUDO and platinum-based chemotherapy, is indicated for the treatment of adult patients with metastatic NSCLC with no sensitizing epidermal growth factor receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK) genomic tumor aberrations.
IMFINZI, in combination with etoposide and either carboplatin or cisplatin, is indicated for the first-line treatment of adult patients with extensive-stage small cell lung cancer (ES-SCLC).
IMFINZI, in combination with gemcitabine and cisplatin, is indicated for the treatment of adult patients with locally advanced or metastatic biliary tract cancer (BTC).
IMFINZI in combination with IMJUDO is indicated for the treatment of adult patients with unresectable hepatocellular carcinoma (uHCC).
There are no contraindications for IMFINZI® (durvalumab) or IMJUDO® (tremelimumab-actl).
Severe and Fatal Immune-Mediated
Adverse Reactions
Important immune-mediated adverse reactions listed under Warnings and Precautions may not include all possible severe and fatal immune-mediated reactions. Immune-mediated adverse reactions, which may be severe or fatal, can occur in any organ system or tissue. Immune-mediated adverse reactions can occur at any time after starting treatment or after discontinuation. Monitor patients closely for symptoms and signs that may be clinical manifestations of underlying immune-mediated adverse reactions. Evaluate clinical chemistries including liver enzymes, creatinine, adrenocorticotropic hormone (ACTH) level, and thyroid function at baseline and before each dose. In cases of suspected immune-mediated adverse reactions, initiate
IMFINZI, as a single agent, is indicated for the treatment of adult patients with unresectable Stage III non-small cell lung cancer (NSCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy.
IMFINZI in combination with platinum-containing chemotherapy as neoadjuvant treatment, followed by IMFINZI continued as a single agent as adjuvant treatment after surgery, is indicated for the treatment of adult patients with resectable (tumors ≥4 cm and/or node positive) NSCLC and no known epidermal growth factor receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK) rearrangements.
IMFINZI, in combination with IMJUDO and platinum-based chemotherapy, is indicated for the treatment of adult patients with metastatic NSCLC with no sensitizing EGFR mutations or ALK genomic tumor aberrations.
IMFINZI, in combination with etoposide and either carboplatin or cisplatin, is indicated for the first-line treatment of adult patients with extensive-stage small cell lung cancer (ES-SCLC).
There are no contraindications for IMFINZI® (durvalumab) or IMJUDO® (tremelimumab-actl).
Important immune-mediated adverse reactions listed under Warnings and Precautions may not include all possible severe and fatal immune-mediated reactions. Immune-mediated adverse reactions, which may be severe or fatal, can occur in any organ system or tissue. Immune-mediated adverse reactions can occur at any time after starting treatment or after discontinuation. Monitor patients closely for symptoms and signs that may be clinical manifestations of underlying immune-mediated adverse reactions. Evaluate clinical chemistries including liver enzymes, creatinine, adrenocorticotropic hormone (ACTH) level, and thyroid function at baseline and before each dose. In cases of suspected immune-mediated adverse reactions, initiate appropriate workup to exclude alternative etiologies, including infection. Institute medical management promptly, including specialty consultation as appropriate. Withhold or permanently discontinue IMFINZI and IMJUDO depending on severity. See USPI Dosing and Administration for specific details. In general, if IMFINZI and IMJUDO requires interruption or discontinuation, administer systemic corticosteroid therapy (1 mg to 2 mg/kg/day prednisone or equivalent) until improvement to Grade 1 or less. Upon improvement to Grade 1 or less, initiate corticosteroid taper and continue to taper over at least 1 month. Consider administration of other systemic immunosuppressants in patients whose immune-mediated adverse reactions are not controlled with corticosteroid therapy.
IMFINZI, as a single agent, is indicated for the treatment of adult patients with unresectable Stage III non-small cell lung cancer (NSCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy (cCRT).
IMFINZI in combination with platinum-containing chemotherapy as neoadjuvant treatment, followed by IMFINZI continued as a single agent as adjuvant treatment after surgery, is indicated for the treatment of adult patients with resectable (tumors ≥4 cm and/or node positive) NSCLC and no known epidermal growth factor receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK) rearrangements.
IMFINZI, in combination with IMJUDO and platinum-based chemotherapy, is indicated for the treatment of adult patients with metastatic NSCLC with no sensitizing EGFR mutations or ALK genomic tumor aberrations.
IMFINZI, as a single agent, is indicated for the treatment of adult patients with limited-stage small cell lung cancer (LS-SCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy (cCRT).
IMFINZI, in combination with etoposide and either carboplatin or cisplatin, is indicated for the first-line treatment of adult patients with extensive-stage small cell lung cancer (ES-SCLC).
IMFINZI, in combination with gemcitabine and cisplatin, is indicated for the treatment of adult patients with locally advanced or metastatic biliary tract cancer (BTC).
IMFINZI in combination with IMJUDO is indicated for the treatment of adult patients with unresectable hepatocellular carcinoma (uHCC).
IMFINZI in combination with carboplatin and paclitaxel followed by IMFINZI as a single agent is indicated for the treatment of adult patients with primary advanced or recurrent endometrial cancer that is mismatch repair deficient (dMMR) as determined by an FDA-approved test.
IMFINZI in combination with gemcitabine and cisplatin as neoadjuvant treatment, followed by single agent IMFINZI as adjuvant treatment following radical cystectomy, is indicated for the treatment of adult patients with muscle-invasive bladder cancer (MIBC).
IMFINZI in combination with fluorouracil, leucovorin, oxaliplatin and docetaxel (FLOT) as neoadjuvant and adjuvant treatment, followed by single agent IMFINZI, is indicated for the treatment of adult patients with resectable gastric or gastroesophageal junction adenocarcinoma (GC/GEJC).
IMFINZI and IMJUDO can cause immune-mediated pneumonitis, which may be fatal. The incidence of pneumonitis is higher in patients who have received prior thoracic radiation.
IMFINZI with IMJUDO and platinum-based chemotherapy can cause immune-mediated colitis, which may be
fatal.
IMFINZI and IMJUDO can cause immune-mediated colitis that is frequently associated with diarrhea.
Cytomegalovirus (CMV) infection/reactivation has been reported in patients with corticosteroid-refractory
immune-mediated colitis. In cases of corticosteroid-refractory colitis, consider repeating infectious workup
to exclude alternative etiologies.
IMFINZI and IMJUDO can cause immune-mediated hepatitis, which may be fatal.
IMFINZI and IMJUDO can cause immune-mediated nephritis.
IMFINZI and IMJUDO can cause immune-mediated rash or dermatitis. Exfoliative dermatitis, including Stevens-Johnson Syndrome (SJS), drug rash with eosinophilia and systemic symptoms (DRESS), and toxic epidermal necrolysis (TEN), has occurred with PD-1/L-1 and CTLA-4 blocking antibodies. Topical emollients and/or topical corticosteroids may be adequate to treat mild to moderate non-exfoliative rashes.
IMFINZI in combination with IMJUDO can cause immune-mediated pancreatitis. Immune-mediated pancreatitis occurred in 2.3% (9/388) of patients receiving IMFINZI and IMJUDO, including Grade 4 (0.3%) and Grade 3 (1.5%) adverse reactions.
The following clinically significant, immune-mediated adverse reactions occurred at an incidence of less than 1% each in patients who received IMFINZI and IMJUDO or were reported with the use of other immune-checkpoint inhibitors.
IMFINZI and IMJUDO can cause severe or life-threatening infusion-related reactions. Monitor for signs and symptoms of infusion-related reactions. Interrupt, slow the rate of, or permanently discontinue IMFINZI and IMJUDO based on the severity. See USPI Dosing and Administration for specific details. For Grade 1 or 2 infusion-related reactions, consider using pre-medications with subsequent doses.
Fatal and other serious complications can occur in patients who receive allogeneic hematopoietic stem cell transplantation (HSCT) before or after being treated with a PD-1/L-1 blocking antibody. Transplant-related complications include hyperacute graft-versus-host disease (GVHD), acute GVHD, chronic GVHD, hepatic veno-occlusive disease (VOD) after reduced intensity conditioning, and steroid-requiring febrile syndrome (without an identified infectious cause). These complications may occur despite intervening therapy between PD-1/L-1 blockade and allogeneic HSCT. Follow patients closely for evidence of transplant-related complications and intervene promptly. Consider the benefit versus risks of treatment with a PD-1/L-1 blocking antibody prior to or after an allogeneic HSCT.
Based on their mechanism of action and data from animal studies, IMFINZI and IMJUDO can cause fetal harm when administered to a pregnant woman. Advise pregnant women of the potential risk to a fetus. In females of reproductive potential, verify pregnancy status prior to initiating IMFINZI and IMJUDO and advise them to use effective contraception during treatment with IMFINZI and IMJUDO and for 3 months after the last dose of IMFINZI and IMJUDO.
There is no information regarding the presence of IMFINZI and IMJUDO in human milk; however, because of the potential for serious adverse reactions in breastfed infants from IMFINZI and IMJUDO, advise women not to breastfeed during treatment and for 3 months after the last dose.
The safety and effectiveness of IMFINZI and IMJUDO have not been established in pediatric patients.
IMFINZI, as a single agent, is indicated for the treatment of adult patients with unresectable Stage III non-small cell lung cancer (NSCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy (cCRT).
IMFINZI in combination with platinum-containing chemotherapy as neoadjuvant treatment, followed by IMFINZI continued as a single agent as adjuvant treatment after surgery, is indicated for the treatment of adult patients with resectable (tumors ≥4 cm and/or node positive) NSCLC and no known epidermal growth factor receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK) rearrangements.
IMFINZI, in combination with IMJUDO and platinum-based chemotherapy, is indicated for the treatment of adult patients with metastatic NSCLC with no sensitizing EGFR mutations or ALK genomic tumor aberrations.
IMFINZI, as a single agent, is indicated for the treatment of adult patients with limited-stage small cell lung cancer (LS-SCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy (cCRT).
IMFINZI, in combination with etoposide and either carboplatin or cisplatin, is indicated for the first-line treatment of adult patients with extensive-stage small cell lung cancer (ES-SCLC).
IMFINZI, in combination with gemcitabine and cisplatin, is indicated for the treatment of adult patients with locally advanced or metastatic biliary tract cancer (BTC).
IMFINZI in combination with IMJUDO is indicated for the treatment of adult patients with unresectable hepatocellular carcinoma (uHCC).
IMFINZI in combination with carboplatin and paclitaxel followed by IMFINZI as a single agent is indicated for the treatment of adult patients with primary advanced or recurrent endometrial cancer that is mismatch repair deficient (dMMR) as determined by an FDA-approved test.
IMFINZI in combination with gemcitabine and cisplatin as neoadjuvant treatment, followed by single agent IMFINZI as adjuvant treatment following radical cystectomy, is indicated for the treatment of adult patients with muscle-invasive bladder cancer (MIBC).
IMFINZI in combination with fluorouracil, leucovorin, oxaliplatin and docetaxel (FLOT) as neoadjuvant and adjuvant treatment, followed by single agent IMFINZI, is indicated for the treatment of adult patients with resectable gastric or gastroesophageal junction adenocarcinoma (GC/GEJC).
Please see Full Prescribing Information including Medication Guide for IMFINZI and IMJUDO.
You may report side effects
related to AstraZeneca products  .
.